Mission Statement
Our goal is to provide unsurpassed quality in a caring and compassionate environment of professionalism and clinical excellence. We hope to exceed your expectations.
What We Do
Types of treatment performed at Advanced Endodontics
- Initial Root Canal Treatment 50%
- Root Canal Re-treatment 40%
- Root Canal Surgery/Apicoectomies 10%
Number of Root Canals (in millions) performed each year in the United States
Estimated number of Root Canals performed each year at Advanced Endodontics of Beverly Hills
Estimated number of Root Canals performed while in Practice

Dr. Jeff Berlin
Jeff received his Doctor of Dental Surgery Degree summa cum laude from the Ohio State University in 1999. After graduation, he continued his training with a certificate of Advanced Education in General Dentistry from the University of California, Los Angeles. Dr. Berlin then returned to the Midwest to specialize in Endodontics as well as earn a Master’s Degree in Oral Biology from the Ohio State University. Dr. Berlin is interested in investigating pain management techniques for dentistry. His Master’s Thesis explored the efficacy of supplemental anesthetic techniques and the systemic effects of anesthetics commonly used in the field of dentistry. Dr. Berlin has published numerous articles in several peer-reviewed journals and he has spent time as a clinical instructor at the UCLA School of dentistry. When not at work, Dr. Berlin enjoys spending time with his family. He is happily married with two beautiful children, Jake and Ellie.

Timely Treatment
Your time is valuable. We make a point to keep to our schedule and to run on time.

Advanced Technology

Clear Communication
Technology used in our practice

Carl Zeiss Surgical Microscopes

Schick CDR Digital radiography

Electric Handpieces

Nickel Titanium Rotary Instruments

Integrated Delivery Systems

Electronic Apex Locators

Learning Center
Root Canal Therapy
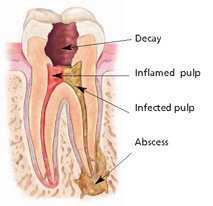
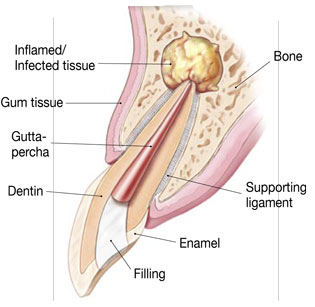
Infection or inflammation of the pulp can be caused by trauma to the tooth, deep decay, cracks, or dental restorations. The infection or inflammation can sometimes be identified sometimes visibly by swelling and sometimes only by symptoms, such as sensitivity to temperature or pain in the tooth and gums. If you experience any of these symptoms, non-surgical root canal therapy helps to eliminate the diseased pulp. This injured pulp is removed and the root canal system is thoroughly cleaned, shaped, and sealed. Endodontic treatment can often be performed in one or two visits and involves the following steps: We first examine and x-rays the tooth, then administers local anesthetic. After the tooth is numb, we will place a small protective sheet called a “dental dam” over the area to isolate the tooth and keep it clean and free of saliva during the procedure. We next make an opening in the crown of the tooth. Very small instruments are used to clean the pulp from the pulp chamber and root canals and to shape the space for filling. After the space is cleaned and shaped, we fills the root canals with a biocompatible material, usually a rubber-like material called gutta-percha. The gutta-percha is placed with an adhesive cement to ensure complete sealing of the root canals. In most cases, a temporary filling is placed to close the opening. The temporary filling will be removed by your dentist before the tooth is restored. After the final visit with us, you must return to your dentist to have a crown or other restoration placed on the tooth to protect and restore it to full function. If the tooth lacks sufficient structure to hold the restoration in place, your dentist may have to place a post inside the tooth.
Root Canal Re-treatment
A tooth may not heal as expected after initial treatment for a variety of reasons:
•Narrow or curved canals were not treated during the initial procedure.
•Complicated canal anatomy went undetected in the first procedure.
•The placement of the crown or other restoration was delayed following the endodontic treatment.
•The restoration did not prevent salivary contamination to the inside of the tooth.
In other cases, a new problem can jeopardize a tooth that was successfully treated.
For example:
•New decay can expose the root canal filling material to bacteria, causing a new infection in the tooth.
•A loose, cracked or broken crown or filling can expose the tooth to new infection.
•A tooth sustains a fracture.
During retreatment, we will re-open your tooth and remove the existing filling materials that were placed in the root canals during the first procedure. We will carefully examines the tooth under microscopic illumination and magnification, looking for additional canals or signs of a new infection. We then remove the sources of infection, clean and shape the canals, and place a new filling material in the root. The opening is then sealed with a temporary filling. Once the tooth heals, a new crown or other restoration is placed on the tooth to protect it.
Root Canal Surgery
The bone naturally heals around the root over a period of months, restoring the tooth back to full function. 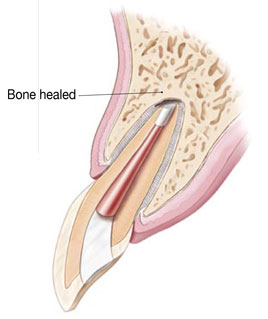
Often, the only alternative to surgery is extraction of the tooth. The extracted tooth must then be replaced with an implant, bridge, or removable partial denture to restore chewing function and to prevent adjacent teeth from shifting. Because these alternatives require surgery or dental procedures on adjacent healthy teeth, endodontic surgery is usually the most biologic and cost-effective option for maintaining your oral health. No matter how effective modern artificial tooth replacements are—and they can be very effective—nothing is as good as a natural tooth. You’ve already made an investment in saving your tooth. The pay-off for choosing endodontic surgery could be a healthy, functioning natural tooth for the rest of your life.
Dental Trauma
Chipped teeth: 
Most chipped or fractured tooth crowns can be repaired either by reattaching the broken piece or by placing a tooth-colored filling. If a significant portion of the tooth crown is broken off, an artificial crown or “cap” may be needed to restore the tooth. If the pulp is exposed or damaged after a crown fracture, root canal treatment may be needed. These injuries require special attention. If breathing through your mouth or drinking cold fluids is painful, bite on clean, moist gauze or cloth to help relieve symptoms until reaching your dentist’s office. Never use topical oral pain medications (such as Anbesol®) or ointments, or place aspirin on the affected areas to eliminate pain symptoms. Injuries in the back teeth often include fractured cusps, cracked teeth and the more serious split tooth. If cracks extend into the root, root canal treatment and a full coverage crown may be needed to restore function to the tooth. Split teeth may require extraction. Dislodged (Luxated) tooth: 
During an injury, a tooth may be pushed sideways, out of or into its socket. We can reposition and stabilize your tooth. Root canal treatment is usually needed for permanent teeth that have been dislodged and should be started a few days following the injury. Medication such as calcium hydroxide may be put inside the tooth as part of the root canal treatment. A permanent root canal filling will be placed at a later date. Children between seven and 12 years old may not need root canal treatment since their teeth are still developing. For those patients, we will monitor the healing carefully and intervene immediately if any unfavorable changes appear. Therefore, multiple follow-up appointments are likely to be needed. New research indicates that stem cells present in the pulps of young people can be stimulated to complete root growth and heal the pulp following injuries or infection.
Knocked out (Avulsed) tooth: 
If a tooth is completely knocked out of your mouth, time is of the essence. Call immediately! Handle the knocked-out tooth very gently, avoiding touching the root surface. When you present to our office, we will carefully evaluate the tooth, place it back in its socket and examine you for any other dental and facial injuries. A stabilizing splint will be placed for a few weeks. Depending on the stage of root development, we may start root canal treatment a week or two later. A medication may be placed inside the tooth followed by a permanent root canal filling at a later date. The length of time the tooth was out of the mouth and the way the tooth was stored before reaching our office greatly influences the chances of saving the tooth. Again, immediate treatment is essential.
Root Fractures: 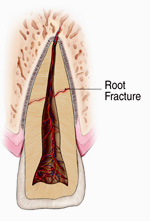
A traumatic injury to the tooth may also result in a horizontal root fracture. The location of the fracture determines the long-term health of the tooth. If the fracture is close to the root tip, the chances for success are much better. However, the closer the fracture is to the gum line, the poorer the long-term success rate. Sometimes, stabilization with a splint is required for a period of time. Cracked teeth manifest with many types of symptoms. Some symptoms include pain when chewing, temperature sensitivities, or pain with the release of biting pressure. It is also common for pain to come and go, making it difficult to diagnose the cause of discomfort. Chewing can cause movement of the cracked pieces of your tooth, and the pulp within the tooth becomes irritated. At the same time, when biting pressure is released, the crack can close quickly, resulting in sharp pain. Eventually, the pulp will become damaged and tooth will consistently hurt, even if you are not chewing. It is possible that cracks can lead to infection of the pulp tissue, which can spread to the bone and gum surrounding the problematic tooth.
Are Root Canals Safe?
The relationship of our teeth and mouth to overall good health is indisputable. Endodontics plays a critical role in maintaining good oral health by eliminating infection and pain, and preserving our natural dentition. A key responsibility of being a dentist is to reassure our patients who are concerned about the safety of endodontic treat- ment that their overall well-being is a top priority. The American Association of Endodontists website (www.aae.org) is the best place for anxious patients to obtain comprehensive information on the safety and efficacy of endodontics and root canal treatment. While plenty of good information is available online from the AAE and other reliable resources, patients sometimes arrive in the dental office with misinformation.This has occurred with the long-dispelled“focal infection theory”in endodontics, introduced in the early 1900s. In the 1920s, Dr.Weston A. Price presented research suggesting that bacteria trapped in dentinal tubules during root canal treatment could “leak” and cause almost any type of degenerative systemic disease (e.g., arthritis; diseases of the kidney, heart, nervous, gastroinestinal, endocrine and other systems). This was before medicine understood the causes of such disease. Dr. Price advocated tooth extraction—the most traumatic dental procedure—over endodontic treatment.This theory resulted in a frightening era of tooth extraction both for treatment of systemic disease and as a prophylactic measure against future illness. Dr. Price’s research techniques were criticized at the time they were published, and by the early 1930s, a number of well-designed studies using more modern research techniques discredited his findings. Decades of research have contradicted Dr. Price’s findings since then. In 1951, the Journal of the American Dental Association published a special edition reviewing the scientific literature and shifted the standard of practice back to endodontic treatment for teeth with non-vital pulp in instances where the tooth could be saved.The JADA reviewed Dr.Price’s research techniques from the 1920s and noted that they lacked many aspects of modern scientific research, including absence of proper control groups and induction of excessive doses of bacteria. More recent research continues to support the safety of dental treatment as it relates to overall systemic health. In 2007, the American Heart Association updated its guidelines on the prevention of infective endocarditis, drastically curbing the indications for premedication for dental procedures and excluding endodontic treatment from dental procedures requiring premedication. In April 2012, the AHA found no scientific evidence linking periodontal disease and heart disease, concluding that heart disease and periodontal disease often coincidentally occur in the same person due to common risk factors of smoking, age and diabetes mellitus. Decades of research contradict the beliefs of “focal infection” proponents; there is no valid, scientific evidence linking endodontically treated teeth and systemic disease. Yet some patients still hear about this long-dispelled theory
- ©2014,American Association of Endodontists, 211 E. Chicago Ave., Suite 1100, Chicago, IL 60611 Phone: 800/872-3636 (U.S. Canada, Mexico) or 312/266-7255; Fax: 866/451-9020 (U.S., Canada, Mexico) or 312/266-9867 Email: [email protected]; Website: www.aae.org
The truth:
•There is no valid, scientific evidence linking root canal-treated teeth and disease elsewhere in the body. A root canal is a safe and effective procedure. When a severe infection in a tooth requires endodontic treatment, that treatment is designed to eliminate bacteria from the infected root canal, prevent reinfection of the tooth and save the natural tooth.
•The presence of bacteria in teeth and the mouth has been an accepted fact for many years. But the presence of bacteria does not constitute “infection” and is not necessarily a threat to a person’s health. Bacteria are present in the mouth and teeth at all times, even in teeth that have never had a cavity or other trauma. Research shows that the healthy immune system takes care of bacteria in a matter of minutes.
•Tooth extraction is a traumatic procedure and is known to cause a significantly higher incidence of bacteria entering the bloodstream; endodontic treatment confined to the root canal system produces much less trauma and a much lower incidence and magnitude of bacteria entering the blood stream.
•There is no adequate replacement for the natural tooth – it should be saved whenever possible. Root canal treatment, along with appropriate restoration, is a cost effective way to treat infected teeth because it is usually less expensive than extraction and placement of an implant. In most cases, endodontic treatment allows patients to keep their natural teeth for a lifetime.
•25 million endodontic treatments are performed every year, safely and effectively. If it were true that root canals caused diseases like cancer, there would be much more information about it available in peer-reviewed scientific publications, and root canals would not be the preferred treatment option to save teeth.
•There is no valid, scientific evidence linking root canal-treated teeth and disease elsewhere in the body. Data showing that “97 percent of cancer patients had root canal treatment” has not been published anywhere. There is no causality between root canals and cancer; just because a person has experienced both doesn’t mean a cause-and-effect relationship exists. As recently as 2013, a study published in a journal of the American Medical Association (JAMA Otolaryngology—Head & Neck Surgery) found that a patient’s risk of cancer doesn’t change after having a root canal treatment; in fact, patients with multiple endodontic treatments had a 45 percent reduced risk of cancer.
•Advancements in medicine, techniques and technologies have made endodontic treatment a more predictable, successful treatment than ever before. Today, digital imaging, rubber dams, rotary instruments, powerful disinfectants and medicated filling materials help ensure successful root canal treatment.
•You wouldn’t cut off your hand if you broke a finger, so why would you extract your natural tooth if it could be saved? Nothing looks, feels or functions like your natural tooth – it should be saved whenever possible. Root canal treatment, along with appropriate restoration, is usually faster and less expensive than extraction and implant surgery. In most cases, endodontic treatment allows patients to keep their natural teeth for a lifetime.
•Claims that root canals are not safe are based on research that’s nearly 100 years old and has long been debunked.
Post-operative Care
A complete report of treatment will be sent to your restorative dentist. Your tooth and surrounding gum tissue may be slightly tender for several days as a result of manipulation during treatment and previous condition of your tooth. This tenderness is normal and is no cause for alarm. This mild discomfort will be relieved by Aspirin, Tylenol, Advil, or the like. Occasionally moderate to severe discomfort may occur. If medication has been prescribed, use it according to the directions (please see our pain management section for further instructions).
If you do not have a prescription for pain medication and feel that you need one, please call the office. Some swelling is also possible. Call the office if more than a slight puffiness occurs. If antibiotics have been prescribed, please take them according to directions until they are all used up. If any other problems develop, please notify the office as soon as possible. In order to protect the tooth against fracture during or immediately after treatment, avoid chewing on the tooth until the final restoration has been placed by your general dentist. You may continue your regular dental hygiene regimen – please continue to brush and floss normally, unless instructed otherwise by our office.
Pain Management following Treatment
Our Recommended therapy for Mild pain relief is:
• 600mg of Ibuprofen (Advil or Motrin) every 4-6 hours for the first 3 days following treatment.
The easiest way to remember how to take the medication is to take 3 (200mg) tablets 4https://advancedendobh.com/wp-admin/post.php?post=2&action=edit#x’s per day at: •Breakfast, •Lunch, •Dinner, and •right before Bed. (every 4-6 hours)
If you were prescribed an antibiotic, you can take it at the same time as the Ibuprofen:
-for Amoxicillin – take it 3x’s per day – at •Breakfast, •Lunch, and •Dinner (but not right before bed)
-for Clindamycin/Penicillin – take it 4x’s per day – at •Breakfast, •Lunch, •Dinner, and •right before bed
-for Biaxin – take it 2x’s per day – at •Breakfast and •Dinner
Moderate to Severe Pain Relief Recommendations: If you are experiencing moderate to severe pain you may need to take the prescribed narcotic medications in addition to taking the Ibuprofen (and/or with prescribed antibiotics).
• Tylenol #3, Vicodin 5/300, or Percocet 5/325 every 4-6 hours while the pain is significant. You may take these narcotic medications in the following manner:
For moderate pain – take 1 tablet of the prescribed narcotic medication at the same time you take the Ibuprofen
For severe pain – Alternate the medications as follows: You may take each type of medication every 4 hours, alternating at different times throughout the day. Therefore, you will be able to take an analgesic pain medication every 2 hours for a more steady pain relief regimen.
For example:
8:00 am – 600mg Ibuprofen
10:00 am – Either: 1-2 extra-strength Tylenol, or Tylenol #3, or Vicodin 5/300, or Percocet 5/325
12:00 am – 600mg Ibuprofen
2:00 pm – Either: 1-2 extra-strength Tylenol, or Tylenol #3, or Vicodin 5/300, or Percocet 5/325
4:00 pm – 600 mg Ibuprofen
6:00 pm – Either: 1-2 extra-strength Tylenol, or Tylenol #3, or Vicodin 5/300, or Percocet 5/325
8:00 pm – 600mg Ibuprofen
10:oo pm – Either: 1-2 extra-strength Tylenol, or Tylenol #3, or Vicodin 5/300, or Percocet 5/325
This discomfort will usually last 3-5 days – sometimes even as long as a week. We call this an endodontic flare-up. Its what can give root canal treatment a bad name. Even after taking the maximum amount of these mediations, sometimes the pain will still remains significant. Be assured that it will get better with time. Unfortunately, time is sometimes the only cure for pain following root canal treatment. Please call our office if you have any questions or concerns. Our doctors are always available if you need to get in touch with us!!
Get in Touch
If you are interested in scheduling an appointment or just gathering more information, send us an inquiry and we will get back to you as soon as we can!
8920 WILSHIRE BOULEVARD, SUITE 403, Beverly Hills, CA 90211
P: 310-855-0444
F: 310-855-1001
EMAIL: [email protected]
OFFICE HOURS:
MONDAY – FRIDAY 8:00 AM – 5:00 PM
Weekends Closed
Parking Information
Parking is available in our building at a rate of $2.45 per 15 minutes. The maximum daily rate is $19.60. Parking is not validated. Free street parking available in the residential areas surrounding our office building. You may park south of Charleville Boulevard, which is located 1 block south of our office building. You may also look for parking on South LaPeer Boulevard and South Almont Street, also south of the building between Charleville Boulevard and Gregory Way. Please read the posted signs for updated parking requirements, as some streets do require permits for parking and there may be either a 1 or 2 hour time limit. YOU SHOULD NOT PARK ON THE BLOCKS BETWEEN WHILSHIRE AND CHARLEVILLE – This is permit only parking and you will LIKELY be ticketed.
We are here, Suite 403

For Our Partners in Patient Care
Download Our Referral Card Here
Archived Newsletter Articles
Bi-Annual Newsletters:
A 3D Approach for Treating Acute Pain (winter 2015)
The Standard of Practice in Contemporary Endodontics (Fall 2014)
The Treatment of Traumatic Dental Injuries (summer 2014)
Endodontic Diagnosis (fall2013)
Regenerative Endodontics (spring2013)
Bisphosphonate-Associated Osteonecrosis of the Jaw (fall 2012)